Our eosinophilosophy
eos counts in
COPD, ABPA, & EOSINOPHILIC PNEUMONIA
There are several lung conditions in addition to severe eosinophilic asthma in which
eosinophils play an important role, including1,2:
COPD is a respiratory disease characterized by airflow limitation and persistent respiratory symptoms including dyspnea, cough, and sputum production. Airflow limitation in COPD is due to airway and/or alveolar abnormalities, which are often a result of marked exposure to noxious gases or particles, with tobacco smoking being the main risk factor.2 US prevalence is conservatively estimated at ~6.5% of the adult population.3
Blood eosinophils are elevated in some patients with COPD. Increased eosinophils in these patients can lead to the release of inflammatory mediators. Some studies show increased risk of exacerbations in patients with elevated blood eosinophil levels; however, other studies show no relationship.2
EOS counts in COPD treatment considerations

Blood eosinophil levels provide guidance for the use of inhaled corticosteroids (ICS) to help prevent exacerbations. Several studies have shown that blood eosinophil counts help predict how well adding ICS to bronchodilator therapy will help prevent exacerbations.2 ICS has little to no effect in COPD patients with lower eosinophil counts of <100 cells/μL.2
Counts of >300 cells/μL can be used to identify patients who
will benefit the most from adding ICS to their bronchodilator
therapy2
Patients with blood eosinophils <2% were found to have an increased risk of developing pneumonia, and therefore this threshold may also be considered in treatment decisions.2
ABPA is an eosinophilic lung condition caused by a hypersensitivity reaction to fungus Aspergillus fumigatus, typically occurring in patients with asthma or cystic fibrosis.1,4,5 ABPA is a subset of allergic bronchopulmonary mycosis (ABPM) and includes hypersensitivity reactions to Aspergillus fumigatus, other Aspergillus species, and other filamentous fungi.4,6 Prevalence of ABPA is estimated to be approximately 2.5% in adult patients with asthma, and approximately 1-15% in patients with cystic fibrosis.7
EOS counts in ABPA diagnosis

Diagnostic criteria for ABPA/ABPM without cystic fibrosis4:
Patients must meet 6 or more of the following 10 criteria for diagnosis of ABPA/ABPM:
- Asthma or history of asthma
- Blood eosinophilia (≥500 cells/µL)
- Elevated serum immunoglobulin E (IgE) (≥417 IU/mL)
- Specific IgE for filamentous fungi* or immediate cutaneous hypersensitivity to filamentous fungi on skin test*
- Specific IgG or precipitins for filamentous fungi*
- Filamentous growth in bronchoalveolar lavage (BAL) or sputum cultures*
- Presence of mucus plugs in central bronchi
- History of mucus plug expectoration, or seen on computed tomography (CT) or bronchoscopy
- Fungal hyphae in bronchial mucus plugs
- CT imaging showing high attenuation mucus in the bronchi
- Central bronchiectasis on CT
*Fungi should be identical.
Early diagnosis and treatment of ABPA/ABPM is important for
prevention of long-term tissue damage6
Acute eosinophilic pneumonia is a rare eosinophilic lung disease with an estimated 9.1 cases per 100,000 patient-years. The disease tends to occur more in males than females, and patients are often in their 20s. A history of smoking is common in patients with acute eosinophilic pneumonia.8 The onset of pneumonia occurs within days and may be associated with a change in smoking habits, such as restarting smoking, increasing cigarette number, or recently starting smoking.1,8

Role of eosinophils in acute eosinophilic pneumonia
Although the exact cause of acute eosinophilic pneumonia is unknown, eosinophil activation and recruitment to the lung is thought to occur via T helper 2 (Th2) cell- and group 2 innate lymphoid 2 (ILC2)-mediated immune responses following alveolar or airway epithelial damage from an inhaled antigen. The damage can lead to secretion of interleukin 25 (IL-25), IL-33, and thymic stromal lymphopoietin (TSLP), polarizing Th2 cells and stimulating ILC2. IL-33 is thought to play an important role in this condition, and elevated levels of IL-33, IL-8, and IL-5 have been found in the blood and BAL fluid in patients.8
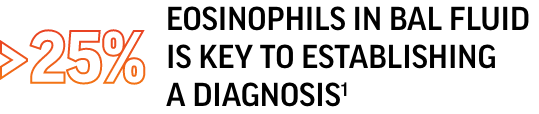
EOS counts in acute eosinophilic pneumonia diagnosis
Modified Philit criteria used for eosinophilic pneumonia diagnosis include1,8:
- BAL fluid eosinophils >25% and/or lung biopsy showing eosinophil infiltration of the lung parenchyma
- Diffuse pulmonary infiltrates (bilateral)
- Hypoxemia
- Acute febrile illness of <1 month
- No known cause of eosinophilic lung disease
Although these criteria are used in diagnosis, there are no formal diagnostic criteria for acute eosinophilic pneumonia8
Blood eosinophilia (>500 cells/µL) in acute eosinophilic pneumonia is rare.8
Chronic eosinophilic pneumonia is a rare eosinophilic lung disease with a reported incidence in the US of 0.5-1.2%. The disease affects females more than males, and the age range of patients tends to be from 30 to 50, although any age can be affected.8 Patients with chronic eosinophilic pneumonia often have a history of asthma and allergies. Patients typically have BAL and blood eosinophilia in addition to elevated immunoglobulin E (IgE).1,8
Clinical manifestations of chronic eosinophilic pneumonia include1,8:
- Prolonged respiratory symptoms (respiratory failure is rare)
- Dyspnea
- Cough
- Wheezing
- Sputum
- Mild hypoxemia or normal blood oxygen
- Low-grade fever
- Loss of appetite and weight loss
EOS counts in chronic eosinophilic pneumonia diagnosis
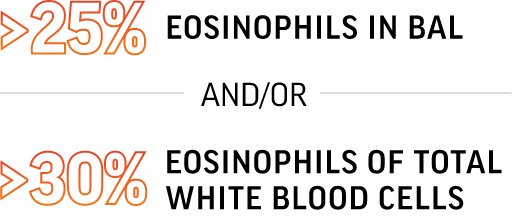
Criteria for chronic eosinophilic pneumonia diagnosis include1,8:
- Respiratory symptom duration >2 weeks
- Chest radiograph showing pulmonary infiltrates
- Infiltrates often have a peripheral predominance
- BAL eosinophilia typically >25%
- Blood eosinophilia (often >30% of white blood cells) and/or evidence of eosinophil infiltration of lungs
- Exclusion of other eosinophilic lung diseases such as ABPA or eosinophilic granulomatosis with polyangiitis (EGPA)
Could it be HES or EGPA?
Chronic eosinophilic pneumonia can have uncommon non-respiratory manifestations (arthralgias, neuropathy, skin and gastrointestinal symptoms) in addition to pulmonary infiltrates and eosinophilia. Also, patients often have a history of allergies and asthma; therefore, differentiating among chronic eosinophilic pneumonia, hypereosinophilic syndrome (HES), and EGPA in some cases may be challenging.1
References:
- Wechsler ME. Pulmonary eosinophilic syndromes. Immunol Allergy Clin North Am. 2007;27(3):477-492.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2024 report. https://goldcopd.org/2024-gold-report/. Accessed July 25, 2024.
- Liu Y, Carlson SA, Watson KB, Xu F, Greenlund KJ. Trends in the prevalence of chronic obstructive pulmonary disease among adults aged ≥18 years - United States, 2011-2021. MMWR Morb Mortal Wkly Rep. 2023;72(46):1250-1256.
- Asano K, Hebisawa A, Ishiguro T, et al. New clinical diagnostic criteria for allergic bronchopulmonary aspergillosis/mycosis and its validation. J Allergy Clin Immunol. 2021;147(4):1261-1268.e5.
- Vitte J, Ranque S, Carsin A, et al. Multivariate analysis as a support for diagnostic flowcharts in allergic bronchopulmonary aspergillosis: a proof-of-concept study. Front Immunol. 2017;8:1019.
- Fukutomi Y, Tanimoto H, Yasueda H, Taniguchi M. Serological diagnosis of allergic bronchopulmonary mycosis: progress and challenges. Allergol Int. 2016;65(1):30-36.
- Data and statistics on aspergillosis. Centers for Disease Control and Prevention. April 24, 2024. https://www.cdc.gov/aspergillosis/statistics. Accessed September 5, 2024.
- Suzuki Y, Suda T. Eosinophilic pneumonia: a review of the previous literature, causes, diagnosis, and management. Allergol Int. 2019;68(4):413-419.
