Our eosinophilosophy
eos counts in
EOSINOPHILIC PNEUMONIA
Acute eosinophilic pneumonia is a rare eosinophilic lung disease with an estimated 9.1 cases per 100,000 patient-years. The disease tends to occur more in males than females, and patients are often in their 20s. A history of smoking is common in patients with acute eosinophilic pneumonia.2 The onset of pneumonia occurs within days and may be associated with a change in smoking habits, such as restarting smoking, increasing cigarette number, or recently starting smoking.1,2

Role of eosinophils in acute eosinophilic pneumonia
Although the exact cause of acute eosinophilic pneumonia is unknown, eosinophil activation and recruitment to the lung is thought to occur via T helper 2 (Th2) cell– and group 2 innate lymphoid 2 (ILC2)–mediated immune responses following alveolar or airway epithelial damage from an inhaled antigen. The damage can lead to secretion of interleukin-25 (IL-25), IL-33, and thymic stromal lymphopoietin, polarizing Th2 cells and stimulating ILC2. IL-33 is thought to play an important role in this condition, and elevated levels of IL-33, IL-8, and IL-5 have been found in the blood and bronchoalveolar lavage (BAL) fluid in patients.2
EOS counts in acute eosinophilic pneumonia diagnosis
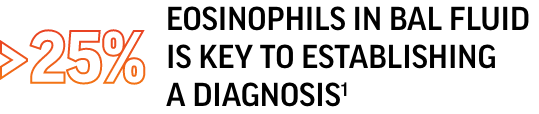
Modified Philit criteria used for eosinophilic pneumonia diagnosis include1,2:
- BAL fluid eosinophils >25% and/or lung biopsy showing eosinophil infiltration of the lung parenchyma
- Diffuse pulmonary infiltrates (bilateral)
- Hypoxemia
- Acute febrile illness of <1 month
- No known cause of eosinophilic lung disease
Although these criteria are used in diagnosis, there are no formal diagnostic criteria for acute eosinophilic pneumonia2
Blood eosinophilia (>500 cells/µL) in acute eosinophilic pneumonia is rare.2
Chronic eosinophilic pneumonia is a rare eosinophilic lung disease with a reported incidence in the US of 0.5-1.2%. The disease affects females more than males, and the age range of patients tends to be from 30 to 50, although any age can be affected.2 Patients with chronic eosinophilic pneumonia often have a history of asthma and allergies. Patients typically have BAL and blood eosinophilia in addition to elevated immunoglobulin E.1,2
Clinical manifestations of chronic eosinophilic pneumonia include1,2:
- Prolonged respiratory symptoms (respiratory failure is rare):
- Dyspnea
- Cough
- Wheezing
- Sputum
- Mild hypoxemia or normal blood oxygen
- Low-grade fever
- Loss of appetite and weight loss
EOS counts in chronic eosinophilic pneumonia diagnosis
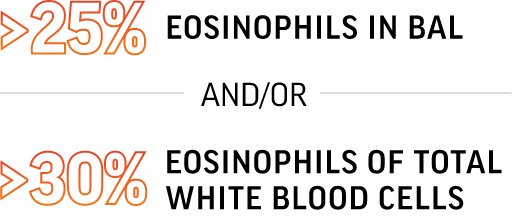
Criteria for chronic eosinophilic pneumonia diagnosis include1,2:
- Respiratory symptom duration >2 weeks
- Chest radiograph showing pulmonary infiltrates
- Infiltrates often have a peripheral predominance
- BAL eosinophilia typically >25%
- Blood eosinophilia (often >30% of white blood cells) and/or evidence of eosinophil infiltration of lungs
- Exclusion of other eosinophilic lung diseases such as allergic bronchopulmonary aspergillosis or eosinophilic granulomatosis with polyangiitis (EGPA)
Could it be HES or EGPA?
Chronic eosinophilic pneumonia can have uncommon non-respiratory manifestations (arthralgias, neuropathy, skin and gastrointestinal symptoms) in addition to pulmonary infiltrates and eosinophilia. Also, patients often have a history of allergies and asthma; therefore, differentiating among chronic eosinophilic pneumonia, hypereosinophilic syndrome (HES), and EGPA in some cases may be challenging.1
